I hope that you are well and that your loved ones are healthy, too.
I am meeting with patients and families via tele-health during this public healthcare situation and plan to keep doing so moving forward. I am using Doxy.me (secure portal) for most folks and recently upgraded bandwidth at home to accommodate working remotely. I’m also open to choosing a platform and format for how we conduct our sessions during this time period.
We will get through this together.
Meeting with patients and their families has been a balm and a blessing during this time, and I will do what I can with you to bring order and calm to whatever place you are at right now. This will involve creativity and flexibility to meet with each other digitally until further notice, and I believe that we can do this effectively and efficiently if we keep working at it together.
Beyond the work changes, my family is going through many of the same challenges others are going through now: children and parents home all day, everyday; working and schooling at the same time, often in the same space; adjusting to a new normal; and, coping with the loss of social activities, celebrations, and milestones we were working towards and looking forward to.
I am in this with all of you.
I am recommending a few things during this time to help us all get through:
I made my own AUggie named “Little B” to keep me company in my home office in the attic.
Be kind to yourself
Practice gratitude
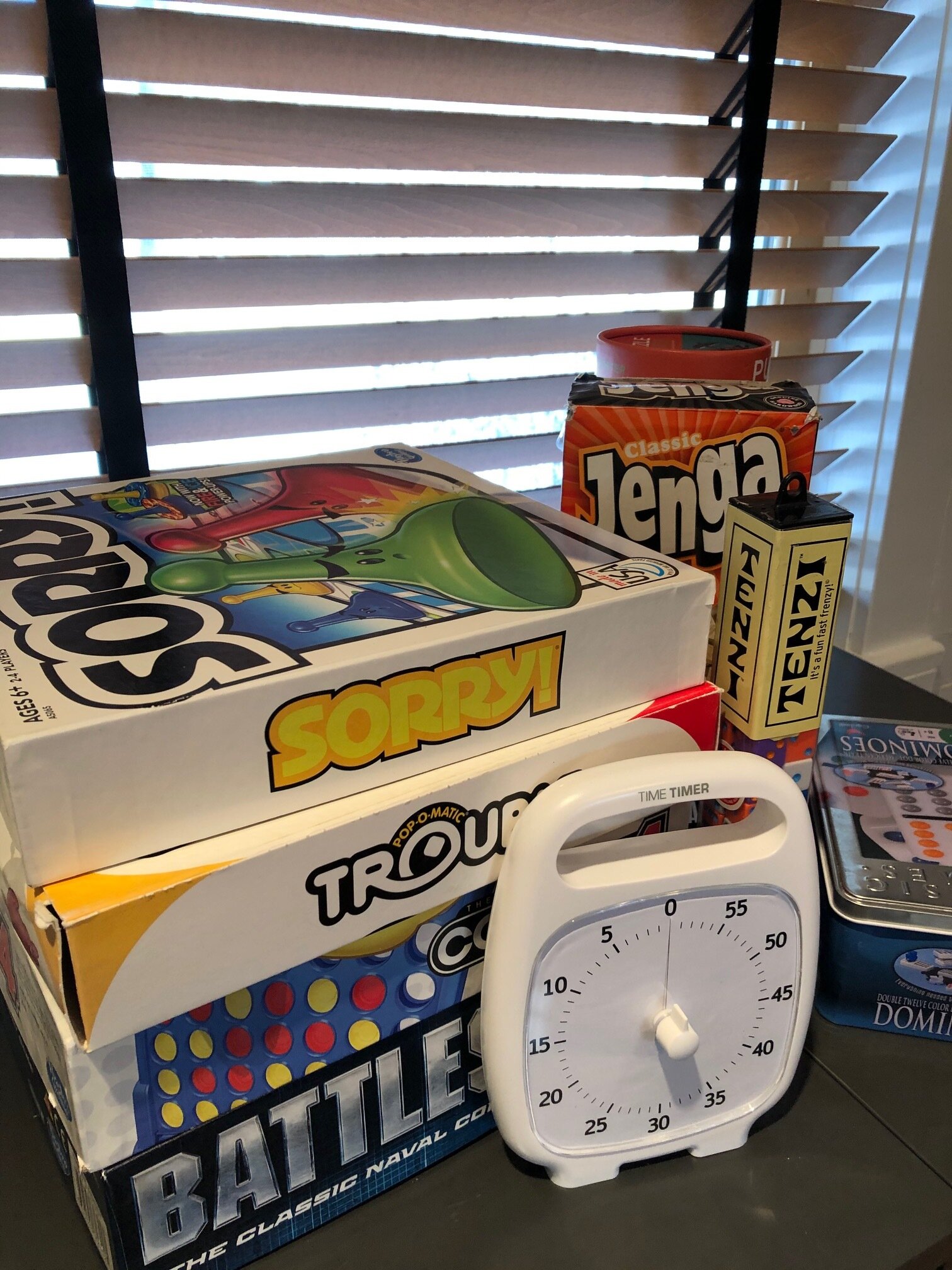
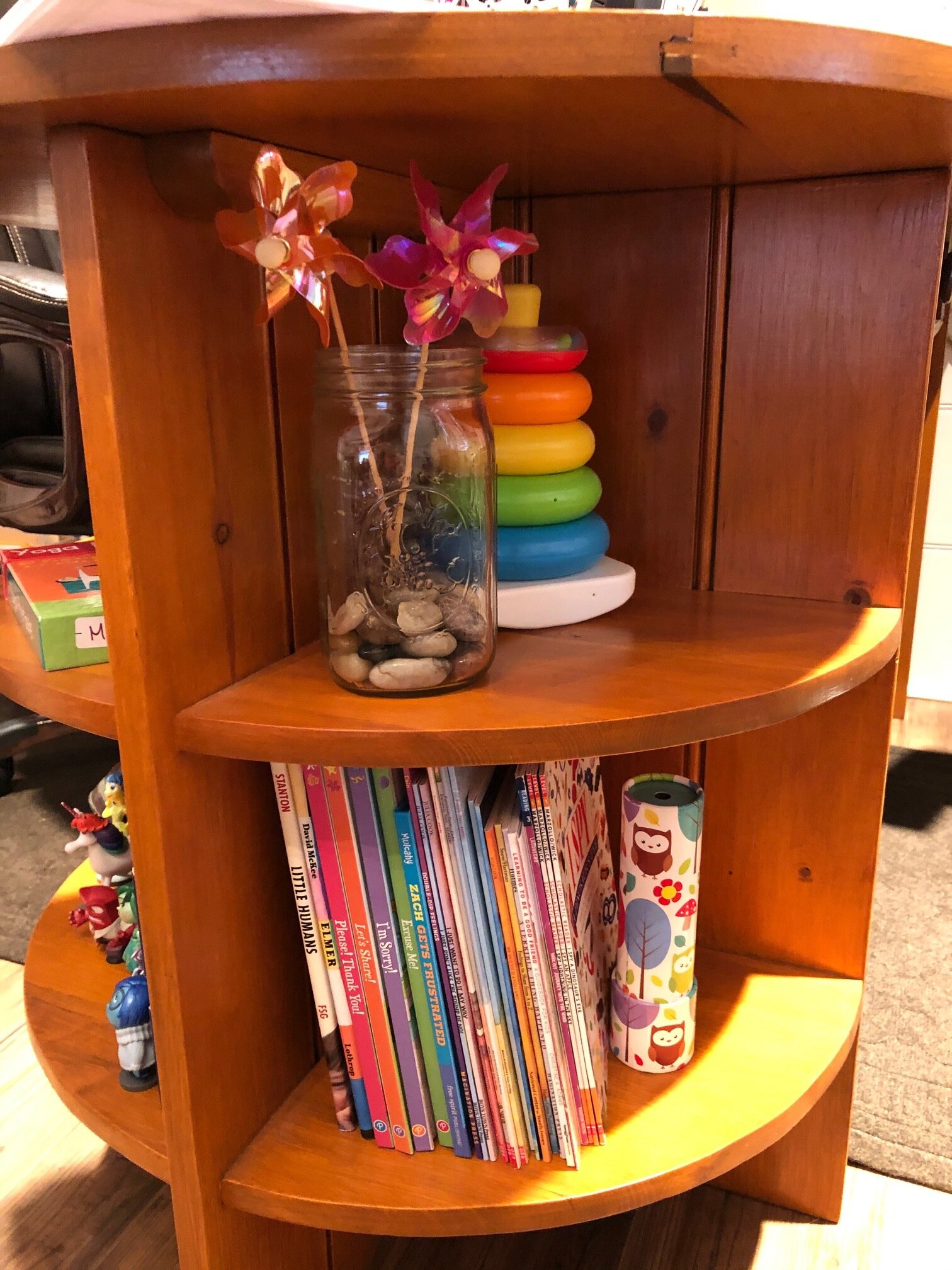
Find rhythm in routines (see image of our dining room/school work space)
Get outside often
Read something fun (see quote below)
Connect with others in your community
For me, an example of #6 is continuing to support AutismUp in my role as Board Member. This means participating in virtual Board Meetings, reading the daily content in @Home with AutismUp they are sending to members and anyone who signs up for the emails, and even participating and sharing in efforts to keep everyone connected.
I see people rising to the challenge of the healthcare situation, and I am amazed at how well everyone is adjusting to this new version of everyday. I encourage you to do less, well and to be patient with the things you cannot hurry and gentle with things that do not move.
“All we have to decide is what to do with the time that is given us.”
J.R.R. Tolkien, The Fellowship of the Ring